Dr. Fernanda De Felice leads research line at IDOR that investigates central nervous system pathologies through biochemical markers
Neuroscience, one of the main and oldest areas of research at the D’Or Institute for Research and Education (IDOR), is a broad field of investigations into the human brain, studying from evolutionary factors such as the origin of feelings, to clinical alterations caused due to congenital, infectious or degenerative diseases.
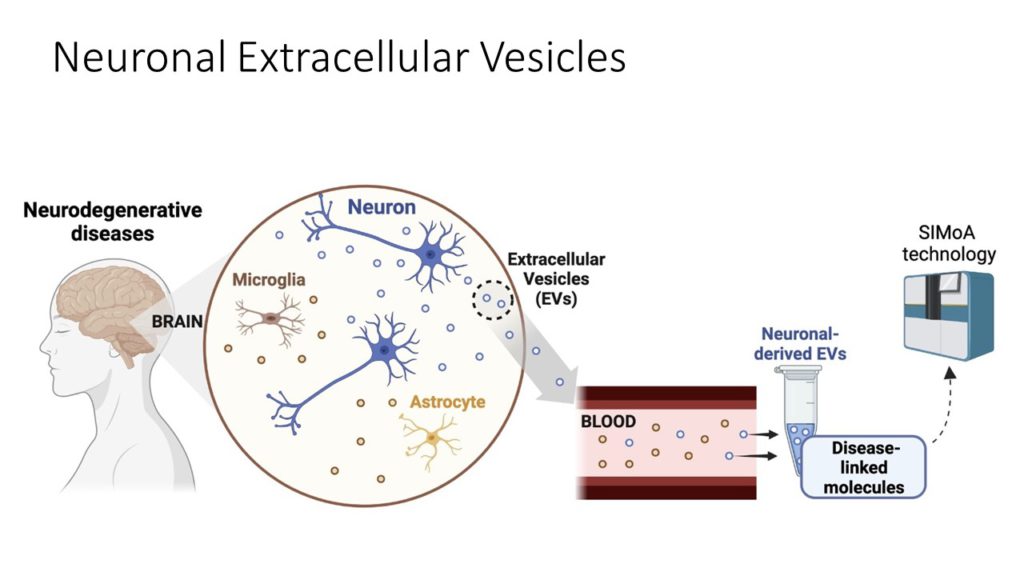
At IDOR, a large segment of this area is dedicated to neurodegenerative processes such as Alzheimer’s Disease and long-term neurological damage caused by COVID-19. All these studies share a common goal: to identify and measure alterations in the Central Nervous System (CNS) that can serve as a pathway to new therapies. Those are the focus of the research line led by Dr. Fernanda De Felice, neuroscientist and molecular scientist at IDOR.
Sitting in her office, with light clothes and a sunny day, it is almost possible to forget that she’s by videoconference, from the other hemisphere of America. The time zone of Southeastern Brazil is similar to that of Ontario, Canada, where De Felice also conducts research at the Queen’s University, in partnership with IDOR. “One of the projects I’ve been working on at IDOR is the search for molecular biomarkers, both for Alzheimer’s disease and the neurological manifestations associated with COVID-19”, she summarizes.
The researcher explains, however, that there is a great challenge in the search for these molecular markers located in the brain: the blood-brain barrier. She exemplifies that, in a neuroimaging study, another investigative line of IDOR, it is possible to see alterations in the brain structure of patients without major obstacles, but to understand chemical scenarios that occur inside the skull, the usual process of sample collection is invasive, as the brain is protected by the blood-brain barrier, which prevents the free molecules traffic between the brain and the blood circulation. In this way, many biomarkers are prevented from leaving the brain environment in large quantities into the bloodstream.